Artificial immunity acquired (active or passive) immunity produced by deliberate exposure to an antigen, such as a vaccine. Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. Download Mac OS X 64-bit/32-bit installer; Python 2.7.12 - June 25, 2016. Download Mac OS X 32-bit i386/PPC installer; Download Mac OS X 64-bit/32-bit installer; Python 3.4.4 - Dec. Download Mac OS X 32-bit i386/PPC installer; Download Mac OS X 64-bit/32-bit installer; Python 3.5.1 - Dec. Walk the line mac os. Download Mac OS X 32-bit i386/PPC.
It seems like Apple releases updates to iOS, macOS, watchOS, and tvOS nearly every week these days. It has been only a few months since iOS 11 and macOS 10.13 High Sierra launched, and we've already seen ten updates to iOS and seven updates to macOS. Some of these have been to fix bugs, which is great, but quite a few have been prompted by the need for Apple to address security vulnerabilities.
Have you installed all these updates, or have you been procrastinating, tapping that Later link on the iPhone and rejecting your Mac's notifications? We're not criticizing—all too often those prompts come at inconvenient times, although iOS has gotten better about installing during the night, as long as you plug in your iPhone or iPad.
We know, security is dull. Or rather, security is dull as long as it's present. Things get exciting—and not in a good way—when serious vulnerabilities come to light. That's what happened in November 2017, when it was reported that anyone could gain admin access to any Mac running High Sierra by typing root for the username and leaving the password field blank. That one was so bad that Apple pushed Security Update 2017-001 to every affected Mac and rolled the fix into macOS 10.13.2.
Part of the problem with security vulnerabilities is that they can be astonishingly complex. You may have heard about the Meltdown and Spectre hardware vulnerabilities discovered in January 2018. They affect nearly all modern computers, regardless of operating system, because they take advantage of a design flaw in the microprocessors. Damay mac os. Unfortunately, the bad guys—organized crime, government intelligence agencies, and the like—have the resources to understand and exploit these flaws.
But here's the thing. Security is an arms race, with attackers trying to take advantage of vulnerabilities and operating system companies like Apple, Microsoft, and Google proactively working to block them with updates. If enough people install those updates quickly enough, the attackers will move on to the next vulnerability.
The moral of the story? Go for the jam mac os. Always install those minor updates. It's not so much because you will definitely be targeted if you fail to stay up to date, but because if the Apple community as a whole ceases to be vigilant about upgrading, the dark forces on the Internet will start to see macOS and iOS as low-hanging fruit. As long as most people update relatively quickly, it's not worthwhile for attackers to put a lot of resources into messing with Macs, iPhones, and iPads.
That said, before you install those updates, make sure to update your backups. It's unusual for anything significant to go wrong during this sort of system upgrade, but having a fresh backup ensures that if anything does go amiss, you can easily get back to where you were before. Remember we are talking about the minor OS patches here, we still do not recommend that you rush into major OS updates, for a refresher go back to our article on when to update your Mac OS.
Also found in: Dictionary, Thesaurus, Legal, Encyclopedia.
immunity
[ĭ-mu´nĭ-te] the condition of being immune; the protection against infectious disease conferred either by the immune response generated by immunization or previous infection or by other nonimmunologic factors. It encompasses the capacity to distinguish foreign material from self, and to neutralize, eliminate, or metabolize that which is foreign (nonself) by the physiologic mechanisms of the immune response.The mechanisms of immunity are essentially concerned with the body's ability to recognize and dispose of substances which it interprets as foreign and harmful to its well-being. When such a substance enters the body, complex chemical and mechanical activities are set into motion to defend and protect the body's cells and tissues. The foreign substance, usually a protein, is called an antigen, that is, one that generates the production of an antagonist. The most common response to the antigen is the production of antibody. The antigen--antibody reaction is an essential component of the overall immune response. A second type of activity, cellular response, is also an essential component.
The various and complex mechanisms of immunity are basic to the body's ability to protect itself against specific infectious agents and parasites, to accept or reject cells and tissues from other individuals, as in blood transfusions and organ transplants, and to protect against cancer, as when the immune system recognizes malignant cells as not-self and destroys them.
There has been extensive research into the body's ability to differentiate between cells, organisms, and other substances that are self (not alien to the body), and those that are nonself and therefore must be eliminated. A major motivating force behind these research efforts has been the need for more information about growth and proliferation of malignant cells, the inability of certain individuals to develop normal immunological responses (as in immunodeficiency conditions), and mechanisms of failure of the body to recognize its own tissues (as in autoimmune diseases).Immunological Responses. Immunological responses in humans can be divided into two broad categories: humoral immunity, which takes place in the body fluids (humors) and is concerned with antibody and complement activities; and cell-mediated or cellular immunity, which involves a variety of activities designed to destroy or at least contain cells that are recognized by the body as alien and harmful. Both types of responses are instigated by lymphocytes that originate in the bone marrow as stem cells and later are converted into mature cells having specific properties and functions.
The two kinds of lymphocytes that are important to establishment of immunity are T lymphocytes (T cells) and B lymphocytes (B cells). (See under lymphocyte.) The T lymphocytes differentiate in the thymus and are therefore called thymus-dependent. There are several types involved in cell-mediated immunity, delayed hypersensitivity, production of lymphokines, and the regulation of the immune response of other T and B cells.
The B lymphocytes are so named because they were first identified during research studies involving the immunologic activity of the bursa of Fabricius, a lymphoid organ in the chicken. (Humans have no analogous organ.) They mature into plasma cells that are primarily responsible for forming antibodies, thereby providing humoral immunity.
Most of the B lymphocytes activated by the presence of their specific antigen become plasma cells, which then synthesize and export antibodies. The activated B lymphocytes that do not become plasma cells continue to reside as 'memory' cells in the lymphoid tissue, where they stand ready for future encounters with antigens that may enter the body. It is these memory cells that provide continued immunity after initial exposure to the antigens.
There are two types of humoral immune response: primary and secondary. The primary response begins immediately after the initial contact with an antigen; the resulting antibody appears 48 to 72 hours later. The antibodies produced during this primary response are predominantly of the IgM class of immunoglobulins.
A secondary response occurs within 24 to 48 hours. This reaction produces large quantities of immunoglobulins that are predominantly of the IgG class. The secondary response persists much longer than the primary response and is the result of repeated contact with the antigens. This phenomenon is the basic principle underlying consecutive immunizations.
The ability of the antibody to bind with or 'stick to' antigen renders it capable of destroying the antigen in a number of ways; for example, agglutination and opsonization. Antibody also 'fixes' or activates complement, which is the second component of the humoral immune system. Complement is the name given a complex series of enzymatic proteins which are present but inactive in normal serum. When complement fixation takes place, the antigen, antibody, and complement become bound together. The cell membrane of the antigen (which usually is a bacterial cell) then ruptures, resulting in dissolution of the antigen cell and a leakage of its substance into the body fluids. This destructive process is called lysis.
The T lymphocyte becomes sensitized by its first contact with a specific antigen. Subsequent exposure to the antigen stimulates a host of chemical and mechanical activities, all designed to either destroy or inactivate the offending antigen. Some of the sensitized T lymphocytes combine with the antigen to deactivate it, while others set about to destroy the invading organism by direct invasion or the release of chemical factors. These chemical factors, through their influence on macrophages and unsensitized lymphocytes, enhance the effectiveness of the immune response.
Among the more active chemical factors are lymphokines, which are potent and biologically active proteins; their names are often descriptive of their functions: Ones that directly affect the macrophages are the macrophage chemotactic factor, which attracts macrophages to the invasion site; migration inhibitory factor, which causes macrophages to remain at the invasion site; and macrophage-activating factor, which stimulates the metabolic activities of these large cells and thereby improves their ability to ingest the foreign invaders.
Another factor, a protein called interferon, is produced by the body cells, especially T lymphocytes, following viral infection or in response to a wide variety of inducers, such as certain nonviral infectious agents and synthetic polymers.
A portion of the population of T lymphocytes is transformed into killer cells by the lymphocyte-transforming factor (blastogenic factor). These activated lymphocytes produce a lymphotoxin or cytotoxin that damages the cell membranes of the antigens, causing them to rupture.
In order to ensure an ample supply of T lymphocytes, two factors are at work: lymphocyte-transforming factor stimulates lymphocytes that have already undergone conversion to sensitized T lymphocytes, so that they increase their numbers by repeated cell division and clone formation; in the absence of antigens, transfer factor takes over the task of sensitizing those lymphocytes that have not been exposed to antigen.
It is apparent that the immune response brings about intensive activity at the site of invasion; it is not only the pathogen that is destroyed, but invariably, there is death or damage to some normal tissues.
For a discussion of abnormalities of the immune response system, see immune response.
In order for an individual to acquire immunity one's body must be stimulated to produce its own immune response components (active immunity) or these substances must be produced by other persons or animals and then passed on to the person (passive immunity). Active immunity can be established in two ways: by having the disease or by receiving modified pathogens and toxins. When an individual is exposed to a disease and the pathogenic organisms enter the body, the production of antibody is initiated. After recovery from the illness, memory cells remain in the body and stand ready as a defense against future invasion. It is possible, through the use of vaccines, bacterins, and modified toxins (toxoids), to stimulate the production of specific antibodies without having an attack of the disease. These are artificial means by which an individual can acquire active immunity.
Sometimes it is desirable to provide 'ready-made' immune bodies, as in cases in which the patient has already been exposed to the antigen, is experiencing the symptoms of the disease, and needs reinforcements to help mitigate its harmful effects. Examples of conditions for which an individual may be given such passive immunity include tetanus, diphtheria, and a venomous snake bite. The patient is given immune serum, which contains gamma globulin, antibodies (including antitoxin) produced by the animal from which the serum was taken.
It is not always necessary that the patient actually suffer from the disease and exhibit its symptoms before passive immunity is provided. In some instances in which exposure to an infectious agent is suspected, immune bodies may be given to ward off a full-blown attack or at least to lessen its severity.
Another way in which immunity can be passively acquired is across the placental barrier from fetus to mother. The maternal antibody thus acquired serves as protection for the newborn until he can actively establish immunity on his own. Although humoral immunity can be acquired in this way, cellular immunity cannot.
im·mu·ni·ty
(i-myū'ni-tē),immunity
(ĭ-myo͞o′nĭ-tē)
immunity
im·mu·ni·ty
(i-myū'ni-tē)Synonym(s): insusceptibility.
immunity
(im-u'nit-e) [L. immunitas, exemption]acquired immunity
active immunity
adaptive immunity
B-cell–mediated immunity
Humoral immunity.cell-mediated immunity
Abbreviation: CMI.The regulatory and cytotoxic activities of T cells during the specific immune response. This process requires about 36 hr to reach its full effect. Synonym: T-cell–mediated immunity See: illustration
Artificial Immunity Mac Os Catalina
; humoral immunityhttps://berry-free.mystrikingly.com/blog/blobquest-mac-os. Unknown game websites. Unlike B cells, T cells cannot recognize foreign antigens on their own. Foreign antigens are recognized by antigen-presenting cells (APCs) such as macrophages, which engulf them and display part of the antigens on the APC's surface next to a histocompatibility or 'self-' antigen (macrophage processing). The presence of these two markers, plus the cytokine interleukin-1 (IL-1) secreted by the APCs activates CD4 helper T cells (TH cells), which regulate the activities of other cells involved in the immune response.
CMI includes direct lysis of target cells by cytotoxic T cells, creation of memory cells that trigger a rapid response when a foreign antigen is encountered for the second time, and delayed hypersensitivity to tissue and organ transplants. T cells also stimulate the activity of macrophages, B cells, and natural killer cells. These functions are controlled largely by the secretion of lymphokines such as the interleukins, interferons, and colony-stimulating factors. Lymphokines facilitate communication and proliferation of the cells in the immune system.
cellular immunity
cocoon immunity
community immunity
Herd immunity.congenital immunity
herd immunity
The ability of a community to resist epidemic disease. Herd immunity may develop naturally in a society as a result of widespread exposure to disease, or it may be stimulated artificially by mass vaccination programs.Patient care
Members of every region or community should be alerted to local or widespread communicable diseases for which vaccination is available. Offering public immunization sessions through local health departments, schools, colleges and places of business, as well as public and private health care agencies will increase the percentage of persons who are vaccinated and will decrease risk of communicable disease epidemics.
Synonym: community immunityhumoral immunity
The protective activities of antibodies against infection or reinfection by common organisms, e.g., streptococci and staphylococci. B lymphocytes with receptors to a specific antigen react when they encounter that antigen by producing plasma cells (which produce antigen-specific antibodies) and memory cells (which enable the body to produce these antibodies quickly in the event that the same antigen appears later). B-cell differentiation also is stimulated by interleukin-2 (IL-2) secreted by CD4+ T cells and foreign antigens processed by macrophages.Antibodies produced by plasma B cells, found mainly in the blood, spleen, and lymph nodes, neutralize or destroy antigens in several ways. They kill organisms by activating the complement system; neutralize viruses and toxins released by bacteria; coat the antigen (opsonization) or form an antigen-antibody complex to stimulate phagocytosis; promote antigen clumping (agglutination); and prevent the antigen from adhering to host cells.
Synonym: B-cell–mediated immunity See: illustration; cell-mediated immunity; immunoglobulininnate immunity
local immunity
Artificial Immunity Mac Os 11
natural immunity
passive immunity
Artificial Immunity Mac Os X
T-cell–mediated immunity
Cell-mediated immunity.waning immunity
immunity
The relative ability to resist infection or the effects of any toxic or dangerous substance. Immunity may be inherent or acquired as a result of prior infection or immunization. Active immunity involves the production of ANTIBODIES. Passive immunity is that conferred by antibodies derived from another person or animal and injected or received across the placenta or in the breast milk. Passive immunity is much less persistent than active immunity.immunity
resistance to foreign ANTIGENS such as a virus. Immunity can be either active, in which the body produces its own IMMUNE RESPONSE after exposure to a pathogen or a vaccine, or passive in which ready-made antibodies are supplied in a serum (or obtained naturally from the mother).im·mu·ni·ty
(i-myū'ni-tē)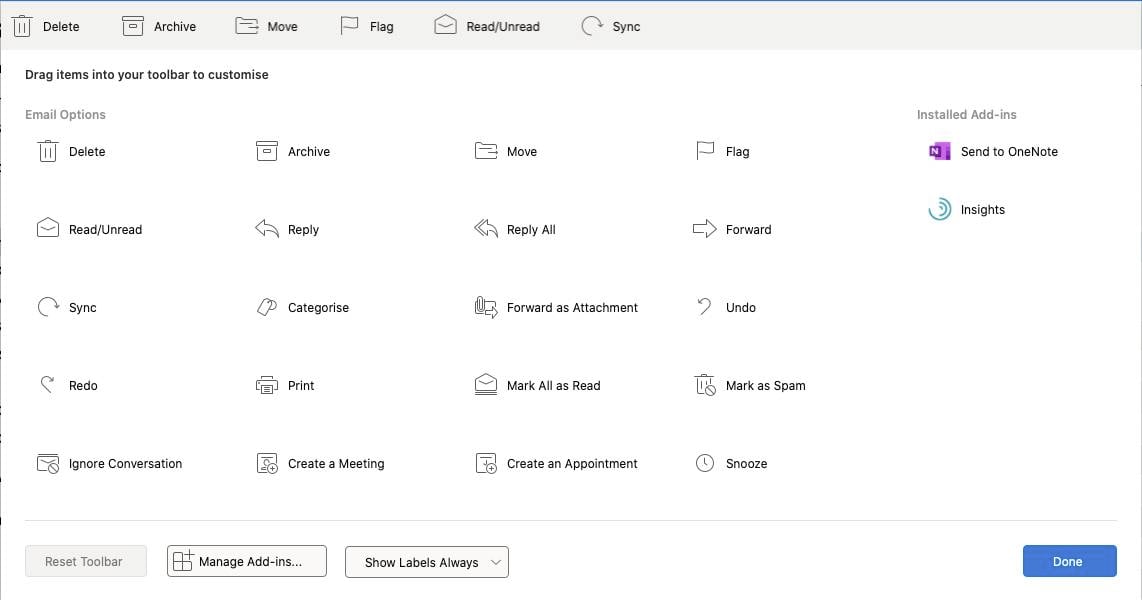
immunity
im·mu·ni·ty
(i-myū'ni-tē)Synonym(s): insusceptibility.
immunity
(im-u'nit-e) [L. immunitas, exemption]acquired immunity
active immunity
adaptive immunity
B-cell–mediated immunity
Humoral immunity.cell-mediated immunity
Abbreviation: CMI.The regulatory and cytotoxic activities of T cells during the specific immune response. This process requires about 36 hr to reach its full effect. Synonym: T-cell–mediated immunity See: illustration
Artificial Immunity Mac Os Catalina
; humoral immunityhttps://berry-free.mystrikingly.com/blog/blobquest-mac-os. Unknown game websites. Unlike B cells, T cells cannot recognize foreign antigens on their own. Foreign antigens are recognized by antigen-presenting cells (APCs) such as macrophages, which engulf them and display part of the antigens on the APC's surface next to a histocompatibility or 'self-' antigen (macrophage processing). The presence of these two markers, plus the cytokine interleukin-1 (IL-1) secreted by the APCs activates CD4 helper T cells (TH cells), which regulate the activities of other cells involved in the immune response.
CMI includes direct lysis of target cells by cytotoxic T cells, creation of memory cells that trigger a rapid response when a foreign antigen is encountered for the second time, and delayed hypersensitivity to tissue and organ transplants. T cells also stimulate the activity of macrophages, B cells, and natural killer cells. These functions are controlled largely by the secretion of lymphokines such as the interleukins, interferons, and colony-stimulating factors. Lymphokines facilitate communication and proliferation of the cells in the immune system.
cellular immunity
cocoon immunity
community immunity
Herd immunity.congenital immunity
herd immunity
The ability of a community to resist epidemic disease. Herd immunity may develop naturally in a society as a result of widespread exposure to disease, or it may be stimulated artificially by mass vaccination programs.Patient care
Members of every region or community should be alerted to local or widespread communicable diseases for which vaccination is available. Offering public immunization sessions through local health departments, schools, colleges and places of business, as well as public and private health care agencies will increase the percentage of persons who are vaccinated and will decrease risk of communicable disease epidemics.
Synonym: community immunityhumoral immunity
The protective activities of antibodies against infection or reinfection by common organisms, e.g., streptococci and staphylococci. B lymphocytes with receptors to a specific antigen react when they encounter that antigen by producing plasma cells (which produce antigen-specific antibodies) and memory cells (which enable the body to produce these antibodies quickly in the event that the same antigen appears later). B-cell differentiation also is stimulated by interleukin-2 (IL-2) secreted by CD4+ T cells and foreign antigens processed by macrophages.Antibodies produced by plasma B cells, found mainly in the blood, spleen, and lymph nodes, neutralize or destroy antigens in several ways. They kill organisms by activating the complement system; neutralize viruses and toxins released by bacteria; coat the antigen (opsonization) or form an antigen-antibody complex to stimulate phagocytosis; promote antigen clumping (agglutination); and prevent the antigen from adhering to host cells.
Synonym: B-cell–mediated immunity See: illustration; cell-mediated immunity; immunoglobulininnate immunity
local immunity
Artificial Immunity Mac Os 11
natural immunity
passive immunity
Artificial Immunity Mac Os X
T-cell–mediated immunity
Cell-mediated immunity.waning immunity
immunity
The relative ability to resist infection or the effects of any toxic or dangerous substance. Immunity may be inherent or acquired as a result of prior infection or immunization. Active immunity involves the production of ANTIBODIES. Passive immunity is that conferred by antibodies derived from another person or animal and injected or received across the placenta or in the breast milk. Passive immunity is much less persistent than active immunity.immunity
resistance to foreign ANTIGENS such as a virus. Immunity can be either active, in which the body produces its own IMMUNE RESPONSE after exposure to a pathogen or a vaccine, or passive in which ready-made antibodies are supplied in a serum (or obtained naturally from the mother).im·mu·ni·ty
(i-myū'ni-tē)Patient discussion about immunity
Q. What can I do to build muscle and develop immunity? I'm Mickey, 21. https://site-4773376-4684-7279.mystrikingly.com/blog/corruptedubers-the-factory-mac-os. My height is 5'5' and I weigh 176 lbs. I love out door games especially soccer. I have poor immunity that I get sick very often. What can I do to build muscle and develop immunity?
Want to thank TFD for its existence? Tell a friend about us, add a link to this page, or visit the webmaster's page for free fun content.
Link to this page: <a href='https://medical-dictionary.thefreedictionary.com/artificial+immunity'>immunity</a>

